SUMMER 2013 CONTENTS
Home
Hiding in plain sight
The environmental factor
Priming the pumps
Debugging Dhaka’s water
Close encounters
How we're crossing paths with disease-bearing pests
Street smarts
Using citizen-scientists to fight for healthier neighborhoods
Beyond hurricane heroics
What Sandy should teach us all about preparedness

DOWNLOAD PRINTABLE
ISSUE (PDF)

Special Report
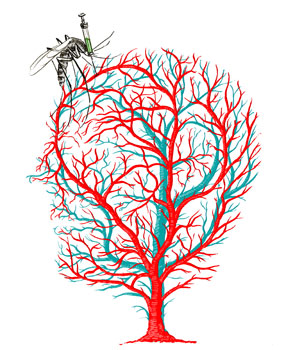
Close encounters
How we’re crossing paths with disease-bearing pests
by Bruce Goldman
Illustration by Daniel Horowitz
Microbes don’t own wings or legs, but they can rent them. Mosquitoes transmit the agents behind malaria and dengue, two of the world’s great tropical scourges. Fleas carry Yersinia pestis, the menace behind the bubonic, pneumonic and septicemic plagues, collectively known in medieval times as Black Death.
While what mosquitoes, fleas, ticks and many other pests carry may vary, they all share a penchant for pawning off their infectious cargo on other animals, including us. In epidemiologic parlance, they’re vectors, from the Latin word meaning “carrier.”
Still, it takes two to tango. For every biter, there has to be a bitee. “We also come to them,” says Eric Lambin, PhD, a Stanford professor of environmental earth system science who calls himself a “landscape epidemiologist.” He tracks, among other things, how our shifting land-use patterns may be rendering us more (or less) prone to vector-borne diseases.
For the past eight years, Lambin, a senior fellow at the Woods Institute for the Environment, has been combining satellite mapping with house-to-house surveys and using computer analysis to crunch all the data thus obtained. The results — reports of the “spatialization” of risk factors for disease spread by animals — could lead to more precise predictions of infectious threats and help guide policymakers in infrastructure and emergency-response planning.
This matters because human activities are modifying large areas of the Earth, causing formerly cryptic pathogens to seemingly pop up out of nowhere. “Epidemiological approaches have often assumed the environment to be an unchanging space,” says Lambin. But that’s not the case.
New diseases have been emerging from swamps, forests and riversides at a rate of about one a year over the past four decades, according to the World Health Organization, which carefully tracks them. We have no genetically based resistance to these new diseases. Meanwhile, long-dormant epidemics have been awakening from their slumber, and some of those aren’t exactly a walk in the park, either.
Not only landscapes but our connection to those landscapes have been transformed by hunting, farming and trading, not to mention high-speed transportation, global migration, urbanization, suburbanization and outdoor recreation: in short, civilization. Any change we make in where we go and when we go there in our daily lives can put us in some vector’s path.
To get a more accurate understanding of the bridges that close the transmission gap between the pathogens and us, Lambin, now the George and Setsuko Ishiyama Provostial Professor in the School of Earth Sciences, became one of the first researchers to combine ground-level data with newly available satellite images of Earth in time segments of 10 years — an approach about a dozen other teams now pursue. It’s how he found himself in Thailand eight years ago, peeking in water containers for mosquito larvae and getting the fish eye from opium-poppy farmers.
Zooming in
Mosquitoes don’t pollinate anything. They don’t crowd out even more obnoxious competitors. Their only known utility is as food for other animal species about which the best that can be said is that they eat mosquitoes. Mosquitoes stink.
But each species of mosquito stinks in its own way. Mosquitoes of the genus Anopheles spread malaria. Those of the genus Aedes transmit dengue fever.
By far the world’s most ravaging tropical parasitic disease is malaria. According to WHO, in 2010 there were some 219 million clinical cases of malaria and an estimated 660,000 deaths, mostly among African children.
Dengue fever, also transmitted by mosquitoes, is a flulike disease widely spread throughout developing countries. While initial infection often proves asymptomatic or mild, it can be quite severe and multiple infections more so. WHO estimates 50 million cases of dengue infection occur each year.
In rapidly developing parts of the world, widespread land-use changes have had a notable impact on the resident mosquito population. In the mid-2000s, Lambin, in collaboration with colleagues including entomologists and epidemiologists, measured that impact in northern Thailand.
The study’s location was ideal for investigating the relationships between land use, mosquito populations and disease transmission: a region encompassing three provinces in far northwestern Thailand where between 1989 and 2000 large areas of forest were cleared for slash-and-burn farming or for permanent fields (mostly orchards) and intensive irrigation farming. Interestingly, the study showed that the slashing of local forest ecosystems might simultaneously increase some mosquito populations and decrease others, thereby cutting down on one disease while abetting another’s rise.
The investigators collected nearly 800 mosquito larvae in and around seven villages, pairing each sample with a description of its larval habitat, collection date and GPS-derived geographic coordinates accurate to within 10 meters. The researchers also inspected water-filled containers for mosquito larvae, which they preserved in alcohol and sent off to a molecular-analysis lab at the University of Leeds in England to be typed by species.
In each village, Lambin and his colleagues obtained epidemiological data for both malaria and dengue. Nearly 2,000 villagers volunteered blood samples and information on their sex, age, profession, birthplace, daytime and evening locations, housing conditions and use of preventive measures such as window screens and bed nets.
Not everyone was willing to talk, Lambin recalls. “As we were analyzing the satellite images in the hills northwest of Chiang Mai, we were detecting small forest clearings, far away from roads and villages, that were obviously cultivated. We were intrigued by this pattern, but found that whenever we interrogated local farmers about it they would shut down and, sometimes, walk away from the interview. We finally realized that these were opium-poppy fields — a small remnant of the old days when the Chiang Mai area was known as ‘the Golden Triangle.’”
The incidence of malaria was so low that the scientists had to discard their data for that disease. But dengue incidence was climbing. Mosquitoes that transmit malaria need dense forests, which villagers had cut down and replaced with orchards. The ones that transmit dengue breed well (and their larvae thrive) in the standing water found in artificial containers villagers liked to use.
All this info, when crunched, allowed Lambin and his colleagues to develop a conceptual model representing interactions between people, the landscape and mosquitoes. According to the model, halving the density of artificial containers in villages during the wet season could significantly reduce the number of infective bites people would receive.
The model further predicted that improved disease-risk awareness and investments in preventive measures, like window screens and bed nets, could influence disease transmission at least as strongly as changes in mosquito populations. Using such prevention measures could counter even a doubling in total orchard area, resulting in the complete suppression of all bites by dengue-transmitting mosquitoes. (The local health agency subsequently promoted these simple preventive measures, but not many residents of remote, poor areas made changes.)
Lambin’s expertise in tying observations from the sky to what can be seen only at ground level made him an ideal collaborator for a project that was to unfold on an other continent.
Checkerboard jungle
In 2012, the Kenyan Wildlife Service reported, Kenya lost approximately 360 elephants to poaching, up from 289 the year before. But an even bigger threat to big wildlife — and to us — is posed by rising human population densities and the conversion of land for growing crops.
If you look at a satellite image of the Amazon basin, says biology professor Rodolfo Dirzo, PhD, the Bing Professor in Environmental Sciences and director of Stanford’s Center for Latin American Studies, you see dramatic disappearances of forested land. This civilization-driven deforestation is happening in Africa and East Asia as well, Dirzo says.
“But satellite imagery won’t tell you anything about another rapid disappearing act going on in many parts of the world,” he says. “And that is the disappearance of large and medium-sized animals. In the Brazilian Amazon, 15 million big animals are being lost each year.”
This phenomenon is called defaunation. Dirzo has been doing fieldwork for decades, mostly in Latin America and mostly in tropical rainforests where human actions have reduced populations of peccaries, tapirs, giant anteaters, monkeys and jaguars. “When there’s gradual loss of rainforest due to human encroachment, what’s left is often not contiguous. Instead, you have little fragments, remnant islands of forest too isolated to maintain big animals. To be genetically viable, a jaguar population needs to consist of at least hundreds of individuals, and this implies an area of tens of thousands of acres.”
We humans worry more about elephants, zebras, jaguars, camels, tapirs, hippos, giraffes and so forth than about their wimpier little mammalian cousins the rodents or, certainly, even less hirsute species from toads to nematodes. But from a pure health standpoint, does the relative abundance of big mammals actually matter to us?
The answer, it turns out, is yes. Defaunation changes the vegetation.
“Grasses grow, shrubs become more abundant,” Dirzo says. Fewer large mammals also means more little ones. “When the big animals go, the population of small rodents tends to increase. Now throw in human habitation, and you have more grain, more shelter” — and, of course, a lower likelihood of getting stomped on. “Those rodents are about to have a wonderful life!”
Dirzo is the principal investigator for an interdisciplinary research project focused on Kenya. The study involves Lambin as well as Michele Barry, MD, professor of medicine, senior fellow at the Woods Institute and senior associate dean for global health in the School of Medicine.
“Studying how increased animal-human contact can facilitate the transfer of pathogens to humans could have huge public-health ramifications,” says Barry.
At Mpala Research Center in Kenya’s Nanyuki District, researchers from UC-Davis have set up “exclosures” surrounded by electrified fences that prevent a piece of a wildlife preserve in the savannah from being trampled by big animals. This simulates defaunation, Dirzo says. On other “control” patches, large animals are not excluded.
Rat and mouse populations inside the exclosures greatly exceed those in the control plots, says Dirzo, who has invented his own term for this: rodentation. “We estimate a roughly 2.7 times greater abundance of rodents when big animals aren’t around,” he says.
The researchers didn’t come up with that statistic by sitting in an air-conditioned office pecking at a keyboard. Here’s a typical working day in the field: “In the afternoon, we go out to the field with lots of rectangular, aluminum traps baited with, say, peanut butter, and lay those traps on the ground spaced 10 meters apart in a large grid. If a rodent goes in, the trap closes, without harming the animal. Early the next morning, before the sun heats up the traps or ants discover the food inside them, we go check. If there’s an animal in a trap, we note where in the grid that animal was collected.”
Each caught animal is held in brief captivity. The scientists affix to its ear a numbered aluminum tag, so they’ll recognize the rodent if they find it again. They weigh it. They draw blood and send it off to the Centers for Disease Control and Prevention for genetic analysis. Somebody — usually Dirzo — combs the animal for fleas, plopping them into an alcohol-filled container that is sent to a lab in the United States where they can be identified by species. Feces are collected to tell what the animal has eaten and what kinds of internal parasites it’s infected with. The animal is then brought back to the exact spot where it was found, and let go. The next afternoon the scientists lay out traps all over again.
The UC-Davis plots in Nanyuki make for “a fantastic experimental setting,” Dirzo says, “but it doesn’t tell you exactly what you’ll see in real life. To find out, we had to go where defaunation is most intense. And that’s, of course, where humans are.”
Dirzo’s team located a nearby human settlement separated by a river from a big-animal conservancy site teeming with elephants, giraffes, zebras and more. In this much more realistic experimental setting, they repeated their laborious routines. “We also sampled inside homes. Some of our most successful trapping nights have been in homes.”
In the human settlement, the researchers saw a 25-fold increase in rodent densities. “Rodents carry more human disease pathogens than large animals do,” says Barry.
Now Lambin and his colleagues are combining remote-sensing-, field- and lab-based data with household-survey results to figure out which disease from which rodent lurks in what kind of geographic niche. “We’ve found,” he says, “that specific types of land use determine what types of rodent species abound, and we’ve found some of the pathogens tend to be very specific to one rodent species. So, we can make intelligent predictions as to what kind of land use promotes what pathogen.” In other words, they can tell which disease might pop up where.
In a small fraction of samples, the CDC has found serious pathogens including Yersinia pestis, the bacterial strain responsible for Black Death. Black Death pandemics decimated entire continents’ populations several times between the sixth and 19th centuries, frequently killing two-thirds of infected people within four days.
There’s no evidence of these pathogens being transferred to people. Yet.
Next?
This is where the expertise of a Michele Barry, who maintains good contacts with the local and mobile clinics that operate in Kenya, comes to the fore. Whitney Bagge, a graduate student whose advisers include Barry and Lambin, returned last summer from a three-week trip to Kenya, where she searched for cases of human rodent-associated disease and gathered ground-based mapping data to synchronize with satellite-based GPS imagery. In a search for lab-confirmed cases of rodent-caused disease, she also visited private and public clinics, local dispensaries and district-level hospitals and spoke to mobile medical-services providers who bring residents of remote communities to these facilities.
“Yersinia pestis is awful,” says Bagge. “But it’s not just extreme examples that are of concern.” Her medical-facilities legwork in and near Mpala has turned up several reports of a mysterious relapsing malarialike syndrome, marked by prolonged fever and malaise, that tests negative for malaria. “We’re thinking the causal agent might potentially be rodent-borne,” Bagge says.
At the moment, Bagge is back at Stanford assessing the data the study has yielded so far. But once the satellite, human-contact and animal-collection data are analyzed and the links between certain geographical niches, the species of rodents that infest them and the particular pathogens those rodent species carry have been drawn, “ideally we’ll be able to use our analysis to extrapolate beyond the rodent-sampling sites we’ve actually studied to the entire region, and to assemble a ‘risk map’ depicting landscapes with likely higher prevalence of one disease or another. We can use that risk map to easily show people their risk for infection in entering a particular area.”
Rodents haven’t been thought of in this area as sources of diseases, so establishing that connection is important in itself. But they are recognized as a nuisance, so rodent-patrol squads already exist. “Knowing which rodents are prone to carrying serious pathogens and which particular landscape types are most likely to house those rodents could direct those rodent patrols to target these areas, for the sake of public health. That would be immediately helpful to medical professionals on the ground,” Bagge says.
“The big, emerging pandemic pathogens we worry so much about primarily spill over to us from animal reservoirs,” says Barry, citing the Nipah virus, featured (albeit in a fictional form) in the 2011 movie Contagion, as an excellent example. The real-life Nipah virus caused 105 deaths in an outbreak in Malaysia in 1999, and 55 more in India in 2001. “Pig farmers were putting their pigsties under mango trees where asymptomatic but virus-shedding, infected fruit bats were roosting. There was a spillover of bat virus to pigs, and then to pig farmers.”
Nipah is just one name on a long list of emerging pathogens that nobody saw coming and re-emerging pathogens nobody expected to come around again. A combination of intensive field work and satellite imaging may help us get a handle on how we can keep them at bay — and, perhaps, establish public-health procedures responsive enough to get out in front of the pathogen we should always fear the most: Pathogen X, the one we don’t know about yet.
Stanford Woods Institute a hub for environmental research
Healthy people and communities need a healthy planet to sustain them. This fundamental understanding drives Stanford researchers who are seeking out solutions to the world’s most pressing environmental challenges.
Several of the researchers featured in this issue, along with 145 other researchers and faculty members representing all of Stanford’s seven schools — are pursuing environmental solutions as fellows and affiliates of the Stanford Woods Institute for the Environment.
The institute was established in 2006 with a gift from Stanford alumnus Ward Woods, ’64, and his wife, Priscilla, to find ways to protect and nurture our planet, and to develop environmental leaders. The institute’s programs emphasize interdisciplinary research targeting the most critical, complex environmental and sustainability challenges. The institute also convenes global experts and stakeholders to advance informed decisions about important environmental topics.
In June, the institute announced its latest round of grants through its Environmental Ventures Program, which provides seed funding to catalyze research in one or more of the Woods focal areas: climate, ecosystem services and conservation, food security, freshwater, oceans, public health and sustainable development. Each project receives funding of up to $100,000 per year for one or two years. Since the annual program began in 2002, it has awarded more than $7.2 million in seed grants to more than 50 projects. These initial grants have led to $39 million in follow-on funding from other sources.
Read more about these and other Stanford Woods Institute projects.