Plus
Transition point
The unmet medical needs of transgender people
By Tracie White
Photography by Brian Smale
Alice Miller, PhD, lived as a man for most of her life. Her primary care physician agreed to help her become a woman, but first had to learn how.
On a September morning about 10 years ago, Lyman Miller, PhD, showed up for an appointment with his family doctor in Half Moon Bay intending to ask for a prescription for female hormones. He was 57 years old, married for a second time, with two grown children. He stood over 6 feet tall, and sometimes wore a rough beard. And he wanted to become a woman.
His doctor, Lorraine Page, MD, thought she knew Miller fairly well. She knew he was a father and a husband. But she had no idea that since childhood he had felt he was truly female. “I’d never discussed this with any doctor,” Miller says. “It took some psyching up. It was embarrassing. I was nervous.” The doctor, understandably, didn’t have a clue.
“He was a very masculine, confident kind of person,” says Page, who knew Miller worked as an expert in Chinese foreign policy and domestic affairs at the Hoover Institution, a think tank on the Stanford campus. “But this visit, he was kind of awkward. There was some hesitation.” So when Miller mumbled something about wanting to get a prescription for hormones, the doctor assumed he meant testosterone for erectile dysfunction. Other male patients with similar requests had shown the same kind embarrassment. “But why?” she recalls asking. “I can get you a prescription for Viagra for that.”
It took some time, and conversation, but eventually the two came to an understanding. Miller got a prescription for estrogen. And Page headed off to do research. Like most doctors, she knew very little about how to meet the medical needs of a transgender patient, particularly one headed down the road toward transitioning. But she was open to learning. Miller gave her some journal articles about recommended hormone dosages in such cases, and she turned to the Internet.
Page is far from alone in her unfamiliarity with transgender people and their treatment. The word “transgender” itself is often misunderstood. Transgender is an umbrella term that encompasses a range of non-conforming gender behavior, including crossdressers (who derive sexual stimulation from dressing in clothes of the opposite gender), drag queens and drag kings, and transsexuals (who feel their body does not match their innate sense of gender identity). Transsexuals may medically “transition” to the gender that’s right for them; others chose not to and so do not require the cooperation of the medical community.
Transitioning is the process of changing gender, which can take anywhere from a few months to years. Its endpoint can entail simply living openly in the new gender, or undergoing hormone therapy and sex-change surgery, or any variation of these steps.
The problem is that in the United States, most physicians don’t exactly know what treatment for the transgender patient entails. For an untrained professional, it’s a challenge to provide care to a patient with a penis who wants a vagina, or to a patient who has been tortured emotionally by being told she’s a boy when she knows she’s a girl.
General practitioners — the majority of doctors who treat patients in the United States — are equally unprepared to care for those transgender patients after they have begun to take hormones and undergone genital-reconstruction surgery. The lack of medical education on the topic, a near-total absence of research on transgender health issues and the resulting paucity of evidence-based treatment guidelines leave many at a loss.
About 700,000 transgender adults live in the United States, about 0.3 percent of the adult population, estimates Gary Gates, PhD, a demographer at UCLA’s Williams Institute, a gender-identity law and public-policy research group. As no national data on this population exist, Gates relied on two studies by state agencies, one conducted by California and the other by Massachusetts.
As for the need for medical care specific to transgender patients, here too only ballpark figures are available. Internationally known transgender-rights advocate Jamison Green, PhD, estimates that for most of the past 30 years, the number of patients undergoing sex-reassignment surgery remained constant, around 1,000 a year. Recently, though, that figure appears to be creeping up, says Green, based on his informal observations at health-care conferences and conversations with transgender people and practitioners. The growth of community-based transgender health forums is further evidence of interest. These forums have emerged in roughly two dozen cities throughout the country over the past five years. In 2011, the largest, in Philadelphia, drew thousands.
Courtesy of Alice Miller
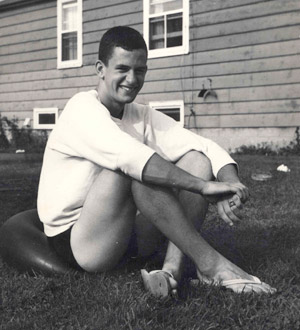
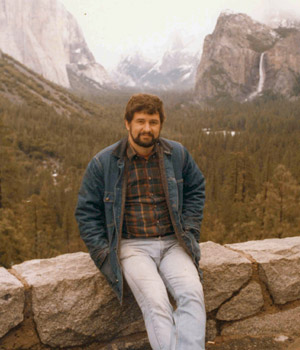 Lyman Miller worked hard at being male. As a young man, he played high school basketball and attended all-male Princeton University. Below: Miller during a trip to Yosemite with Avis Boutell after marrying in 1983.
Lyman Miller worked hard at being male. As a young man, he played high school basketball and attended all-male Princeton University. Below: Miller during a trip to Yosemite with Avis Boutell after marrying in 1983.
More transsexuals are also requiring ordinary medical care that takes into account their uncommon status. Should a male-to-female transsexual be screened for breast cancer? What about a female-to-male? What are the special health risks for transsexuals as a population? These are just a few of the questions.
After decades of silence on the issue, recent land-mark publications have helped bring attention to these growing needs:
In September 2011, medical students at Stanford published a study in the Journal of the American Medical Association on the lack of medical school education on health care for lesbian, gay, bisexual and transgender people. The study, which involved sending surveys to medical school deans across the United States and Canada, found that on average students received less than five hours of training. In addition, the deans made note of the specific lack of education on transgender care.
Earlier that year, on March 31, 2011, the Institute of Medicine had issued “The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding,” calling for more data and research to provide evidence-based care for transgender patients.
And on that same day, the New England Journal of Medicine published one of its first articles on the topic in its clinical practice series, titled “Care of Transsexual Persons” (by endocrinologist Louis Gooren, MD, PhD, of the VU University Medical Center in Amsterdam). The article points to the increasing numbers of transgender people seeking medical care in North America and discusses the need for studies on such topics as the safety of long-term, cross-sex hormone treatment.
When Miller was 13, he came home from school each day, packed a knapsack and headed off to the limestone cliffs behind his home in rural western New York. Alone in the woods, he’d open the bag, pull out a peanut butter sandwich, the hammer and chisel he used to hunt for fossils and, hidden down deep, an old dress of his mother’s taken from the storeroom in his family’s basement.
Miller liked to pull on the dress, then go exploring, digging for fossils and watching for birds. For these few hours, at least, he was free to be the girl he knew he was — a girl he named Alice. Then he would go back home dressed once again in pants, trying hard to be the boy the rest of the world expected him to be. When he turned 14, he put away the dresses hoping that if he tried hard enough to repress his feelings, they would vanish.
He spent much of his life trying to prove his manliness, especially to himself. He played high school basketball, attended an all-male Princeton University, entered the macho world of the CIA as an analyst. He married, had children and never told anyone that as a boy he so wanted to wear a dress like Queen Elizabeth’s golden coronation gown that he secretly made himself a crown. Throughout his life, the shame of his secret self haunted him. He had no idea there was a name for how he felt or that there were others who felt the same. For most of his life he never conceived of the possibility of changing from male to female. Never did it cross his mind to discuss such feelings with a doctor. There was simply no point. Nothing could be done.
It wasn’t until he caught a glimpse of a TV talk show when he was 52 that Miller even heard the word transsexual. And slowly, things began to change.
Transgender people are among the most marginalized individuals in the United States. Invisibility is often seen as a necessity for survival. Fears of eviction and job loss are rampant and well-founded, says Walter Bockting, PhD, professor and coordinator of transgender health services at the University of Minnesota Medical School, who has cared for transgender patients for more than 20 years. On average one person is murdered every month in the United States because of transgender identity, according to the Transgender Legal Defense and Education Fund.
A survey of 6,500 transgender people by the National Center for Transgender Equality published in 2011 found pervasive discrimination in health-care settings. Among the results:
• 19 percent reported being refused care because of their gender status.
• 28 percent said they were subjected to verbal harassment in medical settings.
• 2 percent reported being physically attacked in a doctor’s office.
The survey also found widespread ignorance about the special health needs of transgender people, which can be substantial, even beyond the matter of transitioning. Participants reported rates of HIV infection at four times the national average, with the rates for male-to-female transsexuals the highest: 3.76 percent compared with the general population rate of 0.6 percent. The reasons for this high level are unknown but one likely factor is commercial sex work. Extreme marginalization within society and a resulting lack of self-esteem has led these women worldwide to prostitution for financial support, says Green.
Psychiatric care is perhaps the most desperately needed health service, with 41 percent of respondents reporting they had attempted suicide at least once.
These frightening statistics help explain why someone like Miller might spend years of his life in secret misery hiding his feelings. He was afraid of being called a freak, losing jobs, losing loved ones.
At the age of 52, Miller was teaching at the Johns Hopkins School of Advanced International Studies in Washington, D.C., when one day at home he noticed a Phil Donahue show featuring three women who had once been men referred to as transsexuals.
The show shook him. He was amazed that he wasn’t the only person who felt like he did.
Quietly, he once again began dressing in women’s clothes. It was 1996. He had left the CIA to become a full-time academic. He was divorced with two children, had a well-established career as an expert in Chinese foreign policy, and was married to his second wife, Avis Boutell, whom he loved very much and who knew nothing about the feelings he had been suppressing his entire life.
Two years later, Miller finally spoke the truth. The neighbors glimpsed him in his backyard dressed as a woman, and he told his wife.
“I had tried to live a conventional life,” Miller says. “But there was always this underlying, constant tension. Things just weren’t right. I was aware from the time I was a little kid that I was a girl. I liked wearing girl clothes and playing with girls. I was embarrassed by my genitalia. My body was just wrong.”
Brian Smale 
Most transgender people who transition from one gender to another while married lose their spouse. Boutell says she was confused and shocked, but she loved Lyman and eventually chose to stay with him.
“I knew nothing about transsexuals or anything,” Boutell says. “So we started learning. ... After we decided that Alice should be Alice, it took me a long time to wrap my head around the fact that there is a person outside of gender. ... Alice is a pretty special person. I didn’t want to lose her. I don’t think I could ever love anyone as much as Alice.”
The role of sex in this equation is often confusing for both partners and there are no clear-cut answers.
Avis said, ‘You’re going To be 60. Don’t you want to be on the road to transitioning?’ she told me to go see a therapist.
For Boutell and Miller, both nearing 60, sex became far less important than Miller’s happiness. Miller was still attracted to women, but Boutell never was. “At first, I tried to be attracted to females,” Boutell says. “But I’m just not.” Sex became a non-issue. They just didn’t have it.
Miller started the transition incrementally. After two years passed, he was dressing as a woman at home all the time, but never in public. Boutell could see how much happier he was becoming. She taught him how to wear makeup, gave him manicures. It wasn’t until the couple moved to California and Miller started new jobs there that he finally began to explore the possibility of transitioning full time into life as a woman.
“Avis said, ‘You’re going to be 60. Don’t you want to be on the road to transitioning?’ She told me to go see a therapist.” Miller tracked down one of the few gender-identity specialists on the West Coast, Palo Alto-based Judy Van Maasdam, a social worker who has worked with transgender patients for 30 years, helping them understand the treatments and surgeries, prepare emotionally and find the health-care professionals they need.
For transsexuals seeking sex-reassignment surgery in the United States, preparation usually means following the international guidelines known as the “Standards of Care” set forth by the World Professional Association for Transgender Health, or WPATH.
The standards require patients to give prospective surgeons letters from two therapists confirming a diagnosis of gender identity disorder, as described in the Diagnostic and Statistical Manual of Mental Disorders. And prior to genital surgery, they must live full time as the other sex for at least a year, taking the requisite hormone prescription regularly. While these are non-binding guidelines, most American surgeons refuse to operate unless the patient meets them.
In Miller’s case, the transitioning process meant overcoming the embarrassment and fear of appearing to the world as female. [And from this point on, the story will refer to her as such.] It meant for the rest of her life she would take a daily dose of female hormones to help develop a more womanly figure with breasts and wider hips. It meant 250 hours of electrolysis to remove facial hair — three years of twice-weekly sessions that felt like rubber bands snapping repeatedly against her face — and then enduring the same torture to remove pubic hair in preparation for sex-change surgery. The amount of research, resources, time and money she expended to become a full-fledged woman was astounding. She talked to transgender men and women who had blazed the trail before her, searched websites, joined support groups, found self-help books, tracked down a trained surgeon. The final step, vaginoplasty surgery, she paid for herself at a cost of some $20,000. Insurance coverage wasn’t an option.
Transgender people have been documented throughout history, but the possibility of physically changing the body to match a different gender didn’t exist until the 1930s, when the first sex-change operations were conducted in Europe. The goal was to cure transgender patients of their emotional anguish through surgery and hormone treatments.
The treatment remained on the outskirts of the U.S. medical establishment until the 1960s, when greater funding for medical research and openness about sexuality set the stage for gender dysphoria clinics. The first was at Johns Hopkins University in 1966, followed by programs at the University of Minnesota, UCLA, Northwestern University and Stanford. In 1966, Harry Benjamin, MD — a physician who experimented with hormone treatments — wrote his groundbreaking book, The Transsexual Phenomenon, which provided the initial guidance to health professionals working with this population.
But by the mid-to-late 1980s, the field had declined. Most gender dysphoria programs were shuttered by universities because of a controversial study casting doubt on the programs’ value, shrinking funding and changing social mores. Clinics either moved off campus or disappeared altogether. Many scaled down their services, no longer offering surgery or prescribing hormone therapy. At Stanford, the gender dysphoria program became an independent clinic and moved across the street from the university, where it’s still in existence. Only two U.S. universities — the University of Minnesota and the University of Michigan — still operate gender clinics, and those refer out genital surgeries for transsexuals. In fact, few if any hospitals at U.S. academic medical centers conduct the surgeries. So where do patients go? Many go to Thailand or Belgium where the costs are lower and the frequency of surgery much higher — two or three a day. If the patient stays in the United States, the surgery will be at one of the hospitals where the few U.S. surgeons trained in genital surgery practice. The male-to-female surgery — called vaginoplasty or vaginal construction — will cost about $20,000 to $30,000. The female-to-male surgery is much more expensive — with variations ranging from $35,000 to $100,000, with results often less than perfect. The way most surgeons describe it, it’s much easier to take away than add on.
Today, as a field of medicine, transgender care is virtually nonexistent. Training for specialists in sex-reassignment surgery is rare, says Gordon Lee, MD, assistant professor of plastic and reconstructive surgery at Stanford. “It’s not taught in surgical residencies. Medical schools and students know nothing about it. It is done by a few surgeons at a few locations. Not a lot will publicize that they do this surgery. There’s a stigma about doing it.”
And in the United States, scarcely any research has been conducted over the past 30 years.
There are signs of improvement, in part because of pressure from the transgender community and their advocates, and in part because of recognition by the medical establishment of the need. With more exposure in the media, on the Internet and in workplaces, the growing acceptance of transgender individuals in general has begun to trickle into the medical world.
“Times have turned,” says Bockting of the University of Minnesota’s transgender health services. “The medical needs of transgender patients are being recognized more so than ever before.” He points to a new residency elective at his medical school, a three-week rotation available to family medicine, psychiatry and ob/gyn residents shadowing physicians who do physical examinations and hormone therapy.
A new push for better education on the topic in medical school reflects the change within the medical field. Much of transgender care has moved from specialty clinics into primary care settings where family doctors are prescribing hormones and providing that first line of treatment.
These doctors are looking for help to treat their patients.
“It’s pretty straightforward,” Bockting says. “With some training and guidance a family doctor can provide this care.”
The March 2011 New England Journal of Medicine article points to WPATH and the Endocrine Society as good sources for treatment guidelines.
Miller has come a long way from that initial embarrassing doctor’s visit 10 years ago. Today, Lyman Miller lives full time as Alice Miller: a 6-foot-1-inch, 67-year-old woman with manly hands and a way of tilting her head to the side when she listens that is utterly female.
Miller has kept a chronology of the steps that led to her transition. It stretches from August 2002, when she first began regular sessions with Van Maasdam, to vaginoplasty surgery at Sequoia Hospital in Redwood City, Calif., on Aug. 31, 2007. It recounts the many steps in between that led to her transition — from applying that first estrogen patch, to filing a petition with the San Mateo County courts to legally change her name, to packing up all her “guy clothes” and donating them to a thrift store.
Miller’s greatest fears, which revolved around telling her children, her wife and her bosses, proved unfounded. When she made her transition, she worked not only at the Hoover Institution but at Stanford’s Department of Political Science and at the U.S. Naval Postgraduate School in Monterey, Calif. All three said they had former employees who had made similar requests. All proved supportive. Her two grown children were surprised, but encouraging. Only Boutell’s son from a previous marriage refused to allow the couple to see his two children, causing Boutell untold grief.
“I should have done it a million years ago,” says Miller, her voice deep but soft, her shoes flat but feminine, all trace of the once-heavy beard, gone. “But I was terrified I would lose my whole life.”
Today, Miller says she has no regrets about transitioning.
“Next to marrying Avis, it’s the best thing I ever did,” she says.
For now, with a lack of evidence-based care and insufficient medical school training, many primary care doctors are still on their own searching the Internet for information, pounding the pavement for experts and asking their transgender patients about what kind of care they need.
It still takes some work and research to track down accurate and helpful information, says Green. But it can be done. He points to new guidelines developed by the University of California-San Francisco for such routine concerns as patient intake forms that the Centers for Disease Control is adopting. In addition to WPATH and the Endocrine Society, the Vancouver Coastal Health website is fairly up to date and helpful, he says.
“It’s not rocket science to provide primary care, including hormones, to transgender or transsexual patients,” says Green, who is himself transgender. “It just takes a little awareness, conscientiousness and a genuine respect for us as human beings.” Physicians should be cognizant that sex-change surgery patients often still carry reproductive organs from before, and these may need continuing medical attention. That’s something that can be easily missed, says Nelson Teng, MD, associate professor of obstetrics and gynecology at Stanford, who has treated several female-to-male transsexuals for endometrial cancer — cancer of the lining of the uterus. “Many male transgender patients still have a uterus and still should see gynecologists.”
For Miller, 2011 was the first year she underwent a full physical as a woman, which included a breast exam and a mammogram. After about five years of female hormones, her prostate had greatly diminished in size. Page, her family doctor, wasn’t sure what to do, so she tracked down a San Francisco surgeon familiar with transgender care who advised her that it was OK to stop the exams. The prostate was too small to worry about.
“You do feel like you are experimenting sometimes,” Page says.
E-mail Tracie White
Physician resources for treating transsexual people
Primary care protocol from UCSF
Standards of care from WPATH
The Endocrine Society’s guidelines