SUMMER 2010 CONTENTS
Home
Transformers
How teaching hospitals could lead medicine’s metamorphosis
No holes barred
Interest grows in using natural openings for surgery
The healing hand
Putting the physical back in the physical exam
Take the tube
Mass transit for lab samples
Code green
New hospitals blend healing and conservation
On the record
The nation’s health information technology leader on the future of patient data

DOWNLOAD PRINTABLE
ISSUE (PDF)

Special Report
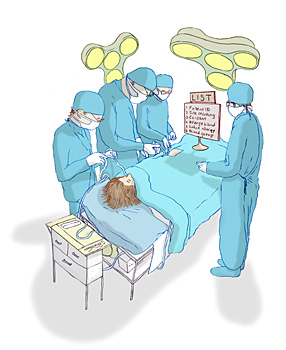
Check please
Using lists to avoid medical mistakes
Illustration by Leif Parsons
On Oct. 30, 1935, the U.S. Air Corps’ chief test pilot was at the controls of a prototype of the B-17 bomber, the Flying Fortress.
He took off, climbed to 300 feet, then stalled and crashed. The pilot and another man died, and others were seriously injured.
What caused the crash? An oversight. Just one skipped step in the long series of take-off procedures: No one had unlocked the newly installed “gust lock,” which kept the craft’s movable control flaps in place while it was parked. Pre-flight checklists became the rule.
Today pilots still use checklists. Construction managers for skyscrapers use them too. And now surgeons are beginning to use them to improve patient safety. Checklists may be foreign to the culture of most operating rooms around the world, but that’s changing.
It’s hard to argue with the logic of checklists. The World Health Organization launched an international push for surgical safety checklists in 2007 and published results of a study trumpeting their value last year. The study of eight hospitals in developed and developing countries, published in the New England Journal of Medicine, found that checklists reduced surgical complications by more than one-third.
As a result of the WHO campaign, led by Stanford University alum Atul Gawande, MD, more than 3,400 hospitals and health-care facilities in 120 countries have either pledged to try the checklist or are using it regularly. In the United States, Medicare’s decision to stop reimbursing hospitals for preventable errors has stoked interest throughout the country.
Last year, Stanford Hospital became one of the first U.S. hospitals to make a full commitment to the pre-surgery checklist; this year, the hospital extended that requirement to all invasive procedures. Government officials in Canada, the United Kingdom and 19 other countries are also moving toward countrywide checklist use. The Checklist Manifesto, a book extolling the use of checklists in medicine, written by Gawande, is a best-seller.
For surgical teams, going through a safety checklist means that before the first incision, the team’s members will introduce themselves and confirm the patient’s identity, corroborate the procedure’s type and location, and check that the patient has received pre-surgical antibiotics to reduce the risk of infection. The team will make sure it has all the equipment it requires — a transplant surgery can involve 400 items — and talk about any special needs for anesthesia or blood. Before taking the patient to recovery, the team will review the procedure and make note of any issues that might cause later problems.
Before the checklist became mandatory at Stanford, some physicians were already using one, says Stanford Hospital’s chief of staff Bryan Bohman, MD. “But there were physicians who were very recalcitrant at first. Maybe they’d never had a wrong-site surgery, or thought that it was fine for hospitals in less developed countries but unnecessary here, or dismissed the whole thing because it seems silly to introduce yourself to someone you’ve worked with for years,” he says. “But we’re seeing more enthusiasm over time.”
Checklists’ results are persuasive, even at Stanford. Clinicians here added a five-step checklist for the insertion of a central line, a catheter that leads through a vein to the heart — something done hundreds of times daily at the hospital. The average infection rate in the United States is around two insertions per 1,000. With the checklist, the infection rate at Stanford dropped to zero.
— Sara Wykes