Are treatments targeting the wrong cell?
 |
|
This stem cell fuels chronic myelogenous leukemia, a type of cancer. |
|
By AMY ADAMS
![]() SIDEBAR: Cancer/Stem Cell Biology at Stanford
SIDEBAR: Cancer/Stem Cell Biology at Stanford
When Catriona Jamieson, MD, PhD, treats her cancer patients with potentially lifesaving chemotherapies, she knows that the benefits will come at a price. The drugs, which destroy all quickly dividing cells in the body, cause her patients to lose their hair, feel nauseous, develop rashes and, in some cases, lose feeling in their fingertips and toes. And then, despite the treatment, often the cancer disappears only to return.
As a medical resident at the University of British Columbia, Jamieson worried that some of her patients were suffering the debilitating side effects in vain. "I thought we were missing the boat because we were targeting the wrong cell," she says.
She thought the right target was an enigmatic cell first identified by John Dick, PhD, at the University of Toronto. In patients with one type of leukemia, Dick had found a type of cell that kept the cancer thriving -- cells called cancer stem cells. At least in this type of cancer, acute myelogenous leukemia, it seemed that it's this handful of slow-dividing cancer stem cells that a therapy must wipe out to eradicate the disease, not the morass of quickly dividing cells that chemotherapy attacks. Jamieson thought that if cancer stem cells underlie one blood cancer, they might also play a role in others. The trouble was that cancer stem cells were such a recent find no one had devised a way to destroy them or even knew how common they were.
Jamieson's concern brought her to Stanford to work with stem cell research pioneer Irving Weissman, MD, (SM '65) the Karel H. and Avice N. Beekhuis Professor in Cancer Biology. Weissman, the first to isolate blood-forming stem cells in mice and humans, has developed ways of purifying and isolating individual populations of blood cells. Jamieson hoped this expertise would help her pull cancer stem cells out of the blood's potpourri of cell types.
Since Jamieson joined the lab in 2001, Weissman has assembled a team to search for stem cells that underlie cancers of the blood, breast, ovaries, lung, brain and bladder, among others -- making his lab the epicenter of the cancer stem cell hunt. As part of this collective effort between Weissman's lab, James Zehnder's lab in the division of hematology, and colleagues at UCLA and Toronto, Jamieson found the first candidate cancer stem cell, publishing results that hint at how normal cells develop into cancer stem cells. Therapies based on these molecules could reach clinical trials within a few years.
Photo:
Amanda Marsalis |
|
 |
|
A few of the stem cell hunters. L to R: Manja Muijtjens, MS, Catriona Jamieson, MD, PhD, Scott Dylla, PhD, and Laurie Ailles, PhD. |
|
Finding the heart of cancer
The idea that dividing stem cells repopulate cancer came about 40 years ago when researchers noticed that only one in 100 human leukemia cells could propagate in a lab dish. But these cancer stem cells remained in the realm of theory until 1994, when Dick found cancer stem cells in acute myelogenous leukemia, the most common form of leukemia. These cells are the only ones that indefinitely generate new cancer cells to keep the cancer growing.
Questions remained about whether all cancers bulk up through division of just a handful of cells. It took until early last year, when Michael Clarke, MD, a professor at the University of Michigan Medical School in Ann Arbor, discovered stem cells in breast cancer, before the idea of cancer stem cells became widely accepted. Later in 2003, two groups announced finding stem cells in forms of human brain cancer.
"I think that more and more people are coming around and believe that cancers have a self-renewing stem cell population," says Clarke. With each division these stem cells produce one new run-of-the mill cancer cell and one cancer stem cell. The regular cancer cells expand their population through rapid divisions and are the target of most chemotherapy or radiation treatments. But over time these cells lose the ability to divide and eventually peter out. The pool of cancer cells requires constant refilling by the slowly dividing cancer stem cells.
Finding those stem cells is a time-consuming task. They make up only a small percentage of the entire cancer and lack identifiable features to mark them as stem cells. Jamieson was aided in her quest by a bank of cancer samples being stored by Stanford's hematology department. She was particularly interested in the chronic myelogenous leukemia samples, in part because she had previously helped test chemotherapy drugs for that cancer. The disease affects about one in 100,000 people, starting slowly and invisibly but building to a hard-to-treat acute phase if not caught early.
Jamieson divided the cells from each sample into populations with unique combinations of molecules on their cell surface. She then put an individual cell from each population in a lab dish to see if it could self-renew.
Cells from only one of the populations could multiply and re-establish a colony. Jamieson had found her cancer stem cell.
The next question was what type of blood cell had turned cancerous. This knowledge could provide some early clues about how the cancer forms and therefore how to block that cell's transformation. When she looked carefully at the proteins on the cancer stem cells, Jamieson found they had a lot in common with a group of cells that exist in the noncancerous bone marrow. These normally divide to produce blood cells called granulocytes and macrophages, important components of the immune system.
Jamieson says that the nature of these precursor cells took researchers by surprise. Researchers had assumed that cancer stem cells would arise from normal adult stem cells that accumulated cancer-causing mutations. That's because these cells are alone among adult cells in having the ability to self-renew. In contrast, Jamieson's cancer stem cells started life as adult cells capable of only a limited number of divisions before death. This was the first hint that the self-renewal pathway could be reactivated in adult cells, or that thwarting that conversion could block cancer.
Another surprise has to do with how chronic myelogenous leukemia develops. The disease is normally caused when chromosomes 9 and 22 swap ends. This trade fuses genes coding for two different proteins into a single unit that makes a cancer-causing protein called BCR-ABL. Jamieson says that blood-forming stem cells in people who go on to develop chronic myelogenous leukemia carry the swapped chromosomes and make BCR-ABL, but for some reason those cells don't become cancerous. Why the adult granulocyte/macrophage progenitor cell is alone in its cancerous fate when the mutation is present in all blood cells remains a mystery, Jamieson says.
Having found the cancer stem cell, Jamieson, Weissman and colleagues were curious what molecular changes allowed that cell to self-renew. One difference they found between normal granulocyte/macrophage progenitor cells and cancer stem cells is a protein called beta-catenin, found in abundance in the nucleus of the cancer stem cells. This protein is well-known to people who study embryonic development, where beta-catenin keeps immature cells in a dividing state. "What's novel is that you have this gene turned on in a mature cell," Jamieson says. Beta-catenin is particularly abundant in people whose cancers resist treatment with the chemotherapy drug Gleevec.
Beta-catenin is part of a signaling pathway kicked off by a protein called Wnt (pronounced "wint"), which has only recently been discovered to play a role in stem cell biology. Last year Weissman and Roeland Nusse, PhD, professor of developmental biology, published a paper in Nature showing that normal blood-forming stem cells require Wnt in their environment in order to self-renew.
As luck would have it, Weissman, who has a long-standing interest in blood-forming stem cells but little knowledge about Wnt, is just down the hall from Nusse, who has built his career studying Wnt signaling. In collaboration with Laurie Ailles, PhD, a postdoctoral scholar in Weissman's lab, the group has been looking for signs that the Wnt pathway also provides cancer stem cells the ability to self-renew.
Ailles says it's too soon to know whether Wnt plays a role in the other cancers being studied by Weissman's lab, but signs hint at the pathway's importance. Proteins that activate the Wnt pathway are commonly mutated in colon cancer, tumors of the hair follicle and in a rare form of brain cancer called medulloblastoma. What's more, a protein called Axin that blocks Wnt signaling also prevented Jamieson's cancer stem cells from propagating.
However, Weissman suspects that many pathways in addition to Wnt may be involved in cancer stem cell self-renewal, not surprising in a disease whose greatest strength as an adversary is its variability. Additional pathways include a gene Clarke and his co-workers at the University of Michigan identified, called Bmi-1, that's needed for self-renewal in both neural and blood-forming stem cells. Weissman says that as members of his lab find cancer stem cells in other types of tumors, more self-renewal proteins are likely to surface.
Shifting focus
Learning how cancer stem cells self-renew is the first step toward drugs that throw a wrench in the cancer propagation machine. That's a much-needed step, according to Ranjiv Sivanandan, MD, a clinical instructor in otolaryngology who, until now, had specialized in surgery for head and neck cancer. He says that although the surgeries for these cancers have become less invasive and chemotherapy and radiation treatments for these cancers have improved, patients live no longer now than they did 30 years ago. "We need a paradigm shift in how we look at and treat cancers," he says.
When Sivanandan learned about Weissman's quest to identify cancer stem cells, he jumped at the chance to participate in the cancer stem cell hunt. He recently extended his two-year fellowship to include an additional year working on this project.
If the work pans out and the group finds stem cells in head and neck cancers and other solid tumors, they will be poised to develop a new breed of cancer drug -- one that targets cells at the heart of cancer. "With the work that's going on now I'm sure there will be clinical studies in the next few years. I'm convinced of that," Clarke says. The trick will be finding drugs that block cancer stem cells without interfering with normal tissue-specific stem cells that replenish the brain, bone marrow, intestines, skin or other organs.
For Jamieson, finding such a drug would ease her misgivings about chemotherapy. If the drugs successfully destroy cancer stem cells, the side effects won't be in vain.
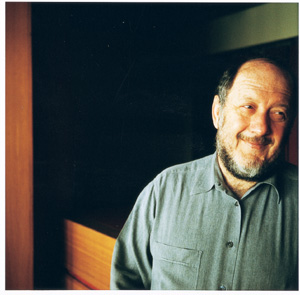
Photo: Leslie Williamson |
|
 |
|
Irving Weissman, director of the Stanford Institute for Cancer/Stem Cell Biology and Medicine. |
|
Cancer/Stem Cell Biology at Stanford
For starters: a collaboration to find cancer stem cells in solid tumors
In December 2002, Stanford created the Institute for Cancer/Stem Cell Biology and Medicine, directed by Irving Weissman, the Karel and Avice Beekhuis Professor of Cancer Biology. Now Weissman has begun putting to use the anonymous $12-million gift that founded the institute. Items on his agenda include:
- Hiring faculty: Scientists who are experts in cancer stem cell biology and in nuclear transfer to create new cell lines are essential for meeting the institute's goal of translating discoveries from stem cell research to disease treatment.
- Creating space: The institute will eventually house five to eight faculty members and their labs, with space for postdoctoral scholars or graduate students who are collaborating with institute scientists but are based in labs outside the institute.
- Achieving NIH Comprehensive Cancer Center designation: This designation will help recruit top faculty members and build a community of cancer expertise that's needed to move basic stem cell research to patient treatment.
- Finding cancer stem cells: A team of 15 basic stem cell researchers and cancer experts from eight departments are collaborating to find cancer stem cells in solid tumors -- the first step to identifying better treatments for these diseases. The burgeoning effort has led to a laboratory space shortage, eased somewhat by the Department of Otolaryngology, which is hosting several cancer stem cell researchers until the institute has its own facility.
Comments? Contact Stanford Medicine at

