 |
||
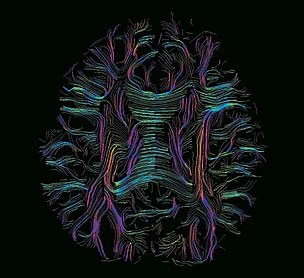
Diffusion-weighted MRI Color-coded white matter fibers reveal the corpus callosum. Appearing as a central band of horizontal blue fibers, the structure connects the brain’s hemispheres. |
||
The brain’s secrets must be handled with care
By Rosanne Spector
Photograph by Roland Bammer
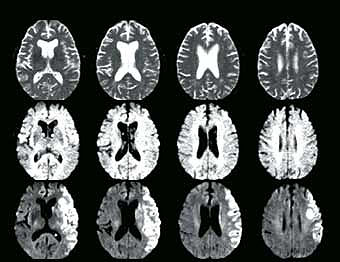
An imaging technique that quickly reveals a brain injury’s size
and location leapt from the lab of radiologist Michael Moseley, PhD,
to hundreds of clinics throughout the world in less than a decade. The
technique, a type of magnetic resonance imaging called diffusion-weighted
MRI, offers improved diagnosis and treatment for stroke.
So what’s next for Moseley and the powerful brain-imaging technique
he developed? Nowadays Moseley, an associate professor in Stanford’s
radiology department, works with colleagues throughout the campus using
the imaging technique to explore human cognition and psychology. He’s
also working with imaging scientists and ethicists to analyze the ethical
issues that arise as a result of neuroimaging findings.
“It won’t be long before neuroimaging will be able to reveal
many of our cognitive strengths and weaknesses,” says Moseley. “This
is exciting for us as researchers. But it makes you stop and think: Will
revealing this information improve someone’s life? Or might it in
some cases change it for the worse?”
As an assistant professor in radiology at the University of California-San
Francisco in 1989, Moseley first used the technique to map the metabolic
changes occurring in very early strokes. He soon realized that the technique,
though not in clinical use at the time, had a huge advantage over standard
clinical imaging tools used on the brain.
“I discovered that I could see strokes only a few hours old,” says
Moseley. He knew that other techniques revealed the damage caused by
strokes many hours or sometimes days after the event, usually too late
to use the information to direct treatment.
Conventional MRI creates images from the variations in materials’ responses
to a strong magnetic field. In medicine, the material usually analyzed
is water, the most abundant element in the body. Instead of simply depicting
water’s concentration in various parts of the brain, Moseley’s
technique went a step further, measuring how fast water diffuses from
place to place.
Stroke patients’ oxygen-starved nerve cells are too impaired to
move water around. As a result, the cells show up clearly using Moseley’s
strategy, though not in regular magnetic resonance images. Moseley first
described this technique’s use in animals in a May 1990 article
in Magnetic
Resonance in Medicine. Since then, the article has been referenced more than
1,500 times by other researchers.
Moseley came to Stanford in 1993 to work with associate professor of
radiology Michael Marks, MD, and neurology professor Greg Albers, MD,
to promote and accelerate the use of diffusion-weighted MRI to treat
stroke.
 |
||
Diffusion-weighted MRI Color-coded white matter fibers reveal the corpus callosum. Appearing as a central band of horizontal blue fibers, the structure connects the brain’s hemispheres. |
||
“I’d say we succeeded. MRI manufacturers now offer commercial
diffusion imaging capability,” says Moseley.
There’s no question that imaging specialists are impressed: In
2000 the International Society for Magnetic Resonance in Medicine granted
Moseley its highest honor, the gold medal.
But in the early 1990s the technique’s value was unrecognized.
Stanford and a few other U.S. medical centers began studying the technique’s
usefulness as a marker of stroke during its acute period — the first
few hours after the event, when clinicians believe there is greatest
potential to help patients.
“We began using diffusion-weighted MRI in the clinical setting
in humans and confirmed a number of hypotheses,” says Marks, Stanford
Hospital’s chief of interventional neuroradiology and director of
neuroradiology at the Stanford Stroke Center. “First, we found the
technique is able to detect acute stroke in a matter of minutes after
its onset. Even at less than an hour, diffusion-weighted MRI can indicate
a stroke. At that time, the brain would still appear normal in images
made by other techniques.”
The greater sensitivity of the technique as compared with conventional
MRI reveals a clearer picture of brain damage and illuminates the cause
of the stroke. Knowing the cause — for instance, a clogged vessel
in the brain versus a blockage in an outer vessel — allows neurologists
to plan treatments more effectively.
Albers, who directs the Stanford Stroke Center, Marks and colleagues
continue to fine-tune their use of the technique to help stroke patients. “We
have found that it is a more sensitive way to detect tissue that is injured
or at risk of injury,” Marks says.
Meanwhile, Moseley is working with collaborators to explore other fields,
in particular, cognition and psychology. His latest studies use diffusion
imaging to trace the movement of water through the brain’s white
matter fibers, which he calls the brain’s thoroughfares. “They’re
the neurochemical pathways connecting the gray matter zones,” he
says.
Moseley is collaborating with many Stanford researchers on his new projects.
They’re discovering that characteristics of the fibers — such
as how they are organized and how robust they are — reveal differences
in individuals’ mental workings. Judith Ford, PhD, associate professor
of psychiatry and behavioral sciences, is investigating schizophrenics’ white
matter wiring. Dolf Pfefferbaum, MD, and Edie Sullivan, PhD, are studying
similar patterns in normal and abnormal aging processes. And John Gabrieli,
PhD, associate professor of psychology, is comparing the brains of dyslexics
and regular readers and has already found clear differences.
Gabrieli’s work shows that the white matter at the left temporal-parietal
junction (located above and a little behind the left ear) may be organized
differently in dyslexics. Even among non-dyslexics, better organization
of the temporal-parietal junction appears to be associated with the ability
to read more quickly.
“This is among some of the earliest examples of diffusion imaging being
applied to cognitive performance,” says Moseley. Being able to image cognitive
centers in the brain offers great potential in understanding the human condition.
It may also open up the possibility for testing remediation programs for cognitive
disorders like dyslexia.”
But the technique’s revelations offer reason for pause. Working
with physicist Roland Bammer, PhD, from Stanford’s radiology department
and bioethicist Judy Illes, PhD, at the Stanford Center for Biomedical
Ethics, Moseley has surveyed research on diffusion imaging of cognitive
performance and discussed some ethical issues raised by its use. They
published their report last year in Brain and Cognition.
Among the questions highlighted:
• What constitutes cognitive impairment on the basis of neuroimaging data?
• How should findings of cognitive impairment be conveyed to the patient
and the family?
• What role should neuroimaging have in selecting students or children into
educational or special therapy programs?
• How can researchers share findings without compromising research subjects’ privacy?
The use of diffusion-weighted imaging for diagnosis and treatment of stroke seems straightforward in comparison with its use on this new frontier. It’s reassuring that Stanford researchers are careful pioneers.
Funding sources for this research:
National Institute of Neurologic Diseases and Stroke,
National Center for Research Resources.
Comments? Contact Stanford Medicine at

