 |
|
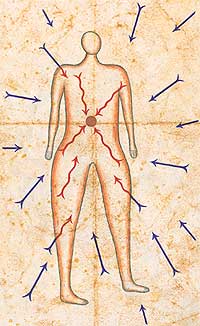
| illustration by philippe weisbecker | |
A quick look at the latest developments from Stanford University Medical Center
![]() Sneeze
away cancer?
Sneeze
away cancer?
![]() Virtual
pelvis reveals ‘inside information’
Virtual
pelvis reveals ‘inside information’
![]() Ken
Melmon, admired clinician, scientist and mentor, dies
Ken
Melmon, admired clinician, scientist and mentor, dies
![]() Zap
brain, ease pain
Zap
brain, ease pain
![]() Communication
says it better
Communication
says it better
![]() A
particle is a particle is a particle
A
particle is a particle is a particle
![]() Do-it-yourself
Genomics
Do-it-yourself
Genomics
Sneeze away cancer?
Researchers at Stanford are giving colds to patients in the hope of curing a deadly disease. In the unusual technique, doctors strive to wipe out cancerous cells in patients’ livers by giving them a shot of modified cold virus.
Thirty-five cancer patients received various doses of a genetically weakened cold virus. The patients suffered flu-like symptoms for about a week, a minor side effect when compared with the nausea, weakness and hair loss that results from standard chemotherapy.
“We want to kill the tumor but not at the expense of the patient,” says Daniel Sze, MD, PhD, assistant professor of radiology.
The 28 patients given the highest virus dose were expected to live about six months. They survived for almost a year, and many of their tumors shrank and appeared to stop producing tumor-associated proteins.
Sze and his colleagues injected the modified virus into an artery leading directly to the liver. Eventually, the virus spread to every cell in the liver, but it infected only cancerous cells.
The modified virus appears to infect tumor cells by taking advantage of a defect common in cancer cells’ version of a protein called p53. “P53 is a DNA spell checker,” Sze explains. “If it finds typos, it shuts down replication.” P53 commands the cell to commit suicide if typos can’t be repaired.
Since the cancer cells have a “broken” p53, they can’t keep the modified virus from invading and replicating.
Future studies will show how effective the treatment is, Sze says. “In this trial, we got a hint that it might actually benefit people with cancer” and that it’s safe. The current study focuses on cancers that originated in the colon and spread to the liver, although Sze adds that it may have use against head and neck, ovarian and pancreatic cancer.
In the next round of trials, Sze plans to clarify how the treatment works and which tumors it effectively fights. — AA
| ![]() Back
to Top |
Back
to Top |
 |
|
| Practicing a pelvic exam with e-pelvis. | |
Virtual pelvis reveals ‘inside information’
Ask the average woman to compile a list of life’s unpleasantries and, chances are, pelvic exams will rank close to the top. And women aren’t alone with that sentiment — the procedure isn’t much of a crowd-pleaser among physicians in training, either.
“Giving a pelvic exam is never something you look forward to,” says Jason Ehrlich, a fifth-year MD/PhD student at the School of Medicine. “It’s awkward to begin with and then you have to wonder, “What do I do?’”
In an effort to answer that question, researchers at the medical school have developed E-Pelvis, a tool that helps students learn how to conduct a pelvic exam. Stanford is the only school in the country to teach students on the device, which simulates the procedure.
Yes, that’s the ovary
E-Pelvis — which Ehrlich describes as “rubber wrapped around things that look like legs” — is an electronic pelvic mannequin attached to a computer monitor. With the help of sensors built into the mannequin, students are able to practice an exam while they and their instructors monitor on a computer screen the location and intensity of touch applied.
Carla Pugh, MD, PhD, developed the device at Stanford four years ago after seeing a need for better training. Second-year students at Stanford typically practice on gynecological teaching associates — female instructors who explain how to give pelvic and breast examinations, guiding students along the way. The associates then offer feedback as students practice. At many other medical schools, however, students practice on patients, and because it’s an internal exam, observing clinicians can’t easily tell how the students are doing.
“When students put their hands inside, you can’t tell where they’re touching and you don’t know if they’re feeling what they’re supposed to,” explains Pugh, a research associate with Stanford University Medical Media and Information Technologies and a surgeon with Kaiser Permanente.
Pugh said she realized she had developed something important while watching students use the device. “The students looked like they were doing the right things, and if I had evaluated them based on this alone, I would have thought they were giving a thorough exam,” she says. “But then I looked at the computer screen and it was like night and day. One student was barely touching anything.”
Less guesswork
“The pelvic exam has been an exam that we’ve assumed students and residents will learn in time — but this device could speed up the process,” Pugh says.
Ehrlich, who used the E-Pelvis for the first time this winter, agrees the device is helpful for both students and future patients. “Being able to simulate techniques and physical movements made it much more comfortable when I had to do it on an actual woman,” he says. “A patient doesn’t want an exam from someone who feels nervous or doesn’t know how to do one, so anything that better prepares clinicians will make the patient more comfortable.” — MB
| ![]() Back
to Top |
Back
to Top |
 |
|
| Ken Melmon, professor of medicine emeritus | |
Ken Melmon, admired clinician, scientist and mentor, dies
Kenneth L. Melmon, MD, professor of medicine emeritus, died April 8, 2002, at his home in Woodside, Calif. A Stanford University alumnus (class of 1956), Melmon had a long, distinguished career at Stanford’s medical school as a devoted teacher and mentor and outstanding clinician and scientist. He died of a heart attack at the age of 67.
As an undergraduate in biology, Melmon decided on a career in medicine and went on to become an eminent clinical pharmacologist, leading administrator and enthusiastic researcher.
His activities ranged from informal mentoring of colleagues to major administrative responsibilities and innovative online resource development.
From 1978 to 1984, he chaired Stanford’s Department of Medicine and served as Arthur L. Bloomfield professor. He also chaired the medical faculty senate and served from 1993 to 2000 as associate dean for postgraduate medical education. In recent years, he was a pioneer in the field of computer-aided education, especially in the creation of SKOLAR, MD, an Internet-based learning system for medical professionals. He was chief medical officer and director of research for e-SKOLAR, an information access startup launched at Stanford in 2000.
Before joining Stanford, Melmon served on the medicine and pharmacology faculty at UC-San Francisco and with the UCSF Cardiovascular Institute from 1965 until 1978. He was also a member of the Institute of Medicine of the National Academy of Sciences.
Memorial contributions may be sent to The Kenneth Melmon Fund, Stanford University School of Medicine, Attn: Jacquelyn Brown, Office of Development, 770 Welch Road, Suite 400, Palo Alto, CA 94304. — JT
| ![]() Back
to Top |
Back
to Top |
 |
|
| Gary Heit calibrates the electrical stimulation to Elaine Pettigrew’s brain. | |
Zap brain, ease pain
A carefully applied jolt of electricity to the brain provided the first pain-free moments for 79-year-old Elaine Pettigrew since her jaw started hurting four years ago. The procedure performed in April at Stanford Hospital was one of just a few of its kind done in the world and the first performed on the West Coast.
“This was a last resort,” says Glen Pettigrew, Elaine Pettigrew’s son. She had tried heavy doses of painkillers and other surgical procedures to ease the constant pain that had sharply limited her quality of life. “When the others didn’t work I started to lose a little hope,” he says.
Pettigrew’s troubles began four years ago when a doctor damaged a nerve in her jaw during an unrelated oral surgery. Since then, Pettigrew has tried a variety of medications and other treatments to block the pain. “I’ve had nerve blocks and I don’t know how many different things,” she says.
Many effective pain medications leave a person groggy, but Pettigrew turned down any drugs that impaired her ability to function. “I drive a car every day and I refused to take something that would affect my driving,” she says, despite pain so easily triggered that the vibration from talking was enough to set it off.
Pettigrew says her primary care physician persistently tried new strategies to approach the problem. “He didn’t give up on me and kept sending me for new treatments.”
Eventually, this led her to Gary Heit, MD, PhD, assistant professor of neurosurgery. Heit saw Pettigrew as a perfect candidate for a new technique that uses brain stimulation to ease pain.
Go for the moving part
The procedure involves a paddle-shaped configuration of four electrodes normally used to stimulate the spinal cord. Heit placed the stimulator on the part of Pettigrew’s brain that controls jaw movement. He then calibrated the device to supply enough current to block pain, but not enough to cause her jaw to move.
Heit said nobody knows for sure why stimulating the movement region impacts pain. A nearby brain region processes sensations from the jaw such as touch or heat; this region would become active if Pettigrew touched her jaw and was active whenever her jaw ached. Crosstalk between the sensory and movement regions keeps these two areas coordinated.
Heit suspects that stimulating the movement region sends a signal both to the jaw and to the sensory region of the brain. Through this process, he believes pain signals from the jaw are blocked, but more study is needed to understand how.
Heit will later run a wire from the stimulator in Pettigrew’s brain to a generator implanted in her upper chest. Pettigrew will be able to flip the device on and off by placing a magnet over her chest.
With her debilitating pain finally relieved, Pettigrew hopes to attend her grandson’s wedding and visit her kids. And she intends to talk — a lot. “Won’t they regret that,” Pettigrew says. — AA
| ![]() Back
to Top |
Back
to Top |
Communication says it better
This spring the office that produces Stanford Medicine magazine changed its name. Formerly the Office of News and Public Affairs, it became the Office of Communication & Public Affairs. “We received suggestions to change our name to acknowledge the multiple roles our staff members play at the medical center,” says Ritch K. Eich, PhD, chief of communication and public affairs. These roles include:
- Producing Stanford Medicine; the weekly Medical Center Report section of Stanford Report; the Medical Staff Update newsletter; and the annual Facts booklet.
- Serving as liaisons to communities involved with the medical center.
- Engaging in 24-hour media-relations efforts.
- Arranging media interviews with medical center experts.
- Supporting the communications efforts of affiliated organizations, such as the VA-Palo Alto Health Care System and University Communications.
The office can be reached by phone at (650) 723-6911 or by fax at (650) 723-7172.
| ![]() Back
to Top |
Back
to Top |
 |
|
| illustration by philippe weisbecker | |
A particle is a particle is a particle
Radiation oncologists can target tumors with greater precision than before thanks to a software code dreamed up by researchers with questions of basic physics on their minds, not medicine.
“The code is an accurate way to calculate how radiation moves through certain media — whether a particle detector or human tissue,” says medical physicist Todd Pawlicki, PhD, assistant professor of radiation oncology.
Now that desktop computers are powerful enough to perform the calculations, Pawlicki and his colleagues in radiation oncology are working to bring the software
into routine use for difficult clinical cases.
Predicting the flow
In the mid-1970s, physicists at the Stanford Linear Accelerator Center developed the Electron-Gamma Shower software to help design shields to protect people from the intense radiation generated by atom-smashing experiments. The software simulates the flow of electrons and photons through matter to reveal where energy is deposited and how many particles travel on through.
But the code’s ability to predict particle activities makes it medically useful too. So just over a decade ago, researchers studying radiation therapy modified the software code to suit their needs. In radiation therapy, medical linear accelerators — room-size, low-energy cousins to SLAC’s 2-mile-long accelerator — create focused X-ray beams that rip apart tumors.
The medical researchers used the software to model the radiation dose coming out of the accelerator and to learn where regular dose estimations went wrong, Pawlicki explains.
By running the calculations to model how radiation moves through patients, the researchers discovered that conventional dose calculations are inexact when the tumor is very small or located in a part of the body made of tissues of greatly varying densities — like the chest, head and neck, says Pawlicki.
Patients might benefit
Now Pawlicki is working with Stanford clinicians including Iris Gibbs, MD, assistant professor of radiation oncology, to learn whether using the Electron-Gamma Shower code would result in fewer risks and complications for patients.
“When we deliver high doses of radiation to small tumors — less than 3 centimeters in diameter — the EGS code may more accurately assess radiation deposition,” says Gibbs.
Their collaboration brings together two complicated disciplines to improve radiation treatment.
“The radiation physics group has very detailed knowledge of these radiation depositions. We rely on their expertise, and they rely on us to determine when it’s clinically relevant to perform these complex calculations,” Gibbs says. — HRW
| ![]() Back
to Top |
Back
to Top |
 |
|
| Esme Coller checks the quality of DNA spots on a microarray created by the Robotic printing machine (at right). | |
Do-it-yourself Genomics
In 1995, the invention of the gene microarray — developed at Stanford by biochemistry professor Patrick Brown, MD, PhD — advanced genomics research tremendously.
These glass slides carrying thousands of DNA “spots” reveal detailed snapshots of which genes are active inside the cell. The technology enables researchers to better understand disease and devise diagnostic methods and treatments.
Seeking Microarrays
Trouble is, relatively few Stanford researchers have had access to the costly technology. The university’s Brown-Botstein Joint Laboratory, co-directed by Brown and genetics professor David Botstein, PhD, has produced gene microarrays for years for themselves and research collaborators, but the lab can’t supply microarrays to all who are interested.
And while a few other labs on campus have set-ups to produce microarrays, that number is small, because the process can be laborious. The only other option is to buy gene microarrays from for-profit companies, but the cost can be out of reach — $500 to $1,000 for each microarray carrying between 10,000 and 20,000 genes.
As a result, researchers whose work could have benefited from microarray technology have been forced to go without.
But no longer. In August 2001, the Stanford Functional Genomics Facility opened to provide gene microarrays to Stanford researchers at the rock-bottom price of $95 for each microarray carrying 40,000 human genes (or 25,000 mouse genes for researchers studying mice). The facility, which already has a one-month waiting list, is a big boost to the university’s research community, says Michael Fero, PhD, the facility’s director.
“The fact that we’re now offering Stanford researchers an entire genome array, essentially at cost, is a pretty radical concept,” he says. “No one else in the country is doing that.”
Since opening, the facility — funded by the school along with grants from Stanford’s Bio-X Program and the National Institutes of Health — has provided more than 5,000 microarrays for departments as diverse as microbiology, surgery and pathology.
The space, located in the Center for Clinical Sciences Research, is dominated by two custom-built robotic machines, each nearly the size of a compact car, that print the results of the microarrays: digital images with a black background and colored spots that show patterns of gene expression occurring within the cells.
Fero and the facility’s six other staff members keep costs low with their do-it-yourself approach. They built the equipment from scratch and offer discounts to researchers who pitch in with some of the prep work.
Fero said this upfront work isn’t difficult and he offers free weekly workshops to teach researchers the necessary steps. “It’s not magic,” he says. “Anyone can do it.” Still, there’s something almost magical about microarrays and the insights they provide. “I think this is pretty gee-whiz stuff,” he says. — SS
| ![]() Back
to Top |
Back
to Top |
Comments? Contact Stanford Medicine at

