A cancer treatment is born of an elusive blood cell few believed existed
By MITZI BAKER
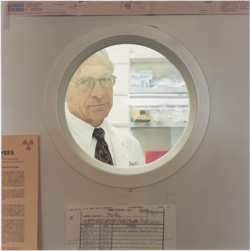
Stewart Loken, a 64-year-old physicist from Berkeley, took a scientific approach to fighting his cancer — he immediately jumped into an experiment. “Science is about having a theory and making measurements to see if that theory is correct,” he says. Three and a half years ago, Loken received a new treatment being tested at Stanford, a new method of blood stem cell transplantation for treating cancers of the blood cells and bone marrow. Loken had chronic lymphocytic leukemia, the most common form of leukemia in adults.
Jeffrey Fisher |
|
 |
|
The method that Stanford researchers tested on Loken aims to retain the desired result of the cell transplant — the killing of the cancerous leukemia cells — without inducing a potentially deadly side effect that often accompanies the procedure. The side effect is graft-versus-host disease, in which the incoming donor cells attack the patient’s body as foreign.
The ability to tease apart the favorable results of a blood cell transfer from the bad seems too good to be true, but 30-odd years of methodical studies in mice back it. “What appealed to me was that there was an underlying theory to this treatment,” says Loken. “To me, much of medical science always appeared to be an oxymoron; it’s more of an art. Here we could really follow scientifically the progress of the treatment, which made me feel confident that this was something we could watch and had scientific validation.”
The irony is not lost on Loken that a tiny white blood cell — the basis of the therapy that restored his ability to endure 100-mile bike rides, scuba dive and kayak — had been the center of a heated decades-long debate in the field of immunology. For many years, most immunologists doubted the cell’s very existence.
Not only have the phantom white blood cells — known as regulatory T cells — now proven their existence, but they’ve become the darlings of immunology researchers worldwide. It’s a heartening success story, proof of the great payoffs that can accrue when scientists follow impulses to unravel scientific mysteries, no matter how unfashionable they are.
“There has been an explosion in interest in the regulatory T cells,” says Samuel Strober, MD, an immunologist who has studied the cells over the last 30 years and has been one of their greatest proponents. “People thought the cells explained nothing, and now they are getting to the point where they try to use them to explain everything.”
“These cells have relevance to almost every immune-mediated disease you can think of,” says Stanford pediatric immunologist Alan Krensky, MD, who becomes the NIH deputy director for the Office of Portfolio Analysis and Strategic Initiatives in July. At Stanford, Krensky looked at regulatory T cell function in human allergies. And he is not alone: Currently, 39 faculty at Stanford include regulatory T cells in some aspect of their work. Researchers at Stanford and in universities worldwide are implicating faulty regulatory T cell function in autoimmune disease, cancer, allergies and asthma.
Backing into a quest
When Strober arrived at Stanford in 1971 as a 31-year-old immunologist, a popular theory held that balance in the immune system was maintained by a cell that could dampen response. It made sense; otherwise a person might, for example, have a cold that went on forever. Such a “response soothing” cell might also play a role in suppressing immune reactions in autoimmune diseases, rejection of organ transplants and cancer. These theoretical peacekeepers of the immune system came to be known as suppressor T cells.
Leslie Williamson |
|
 |
|
|
Strober had no intention of studying these suppressor cells at Stanford. He was interested in organ transplants and, in particular, how to convince the immune system not to reject transplanted organs. Almost immediately, Strober became intrigued by the work that radiologist Henry Kaplan, MD, was doing by manipulating the immune system with irradiation to cure Hodgkin’s disease. When patients were treated using Kaplan’s method, their immune systems became more suppressed. Strober wondered if he could apply this effect to improve his own organ transplant experiments.
Kaplan had worked out a method of irradiating just the lymph nodes, spleen and thymus of a patient rather than the whole body to kill the cancerous cells but preserve the bone marrow. Called total lymphoid irradiation, or TLI, Kaplan’s technique transformed Hodgkin’s disease from a death sentence into one of the most successfully treated cancers.
Strober’s group had already worked out how to transfer a patch of skin from one strain of mouse to another by first giving the skin recipient a blood stem cell transplant from the skin donor. But the transplant sparked an attack of the recipient mouse’s tissues: graft-versus-host disease.
By adding TLI before the transplant, the mice still accepted the grafts but had markedly reduced graft-versus-host disease. “There was no reason to suspect that would happen and it certainly came as a surprise,” says Strober. “I would call that complete serendipity.”
In 1976, Strober, Kaplan and two postdoctoral researchers in their labs published a report of the unexpected resistance to graft-versus-host disease in Science. Shortly after that publication, Strober indicated that this protection was due to suppression of immune responses by a type of cell that became more plentiful relative to other types of T cells following TLI.
But what was this mysterious cell and how could its immune system-soothing qualities be harnessed? Strober spent the next 20 years trying to pin down the answers.
The problem with suppressor cell theories is that no one could find the predicted genes that would make suppressor T cells possible. “The molecular biology didn’t pan out,” says Strober. “It was enough to cause the field to implode.” A rift soon divided the immunologists who believed in the cells and those who didn’t. “At the time the field imploded, at its very low point, probably 90-plus percent of the immunology community didn’t believe that suppressor cells existed,” he says.
Suppressor cells seemed destined for the “immunological waste heap,” agrees C. Garrison Fathman, MD, professor of immunology and rheumatology, whose lab has worked on these cells for the last few years. Meanwhile, Strober and a handful of other immunologists worldwide continued to generate compelling results pointing toward a naturally occurring cell that suppressed immune response.
Throughout the ’80s, Strober presented his findings widely. He says his findings were too out there for other scientists to take seriously. There were no big scenes at meetings, no one calling Strober crazy. “The work that I was doing with these suppressor cells was so off the mark at the time, nobody even paid attention to it. In other words, nobody cared to rebut it,” he recalls. “They felt that it wasn’t even worthwhile responding to the kinds of claims that I was making.”
During this time, one of Strober’s allies at Stanford was genetics professor Leonore Herzenberg, PhD. She looks back with frustration at the way research funding halted when scientists initially failed to turn up genetic evidence of the cells’ existence. “What didn’t make sense was what might be called throwing the baby out with the bathwater,” she says. “People felt it necessary to treat the older data as if it was incorrect or didn’t exist; the baby with the bathwater is that nobody could get funding to study this further and with it was a sullying of the reputation of the people who had worked in this field.”
A shift began to take place in the mid-1990s with a reliable way to identify the cells, which constitute only about 10 percent of the T cells in mice and 10,000-fold less than that in humans. A series of reports resurrected the field, culminating with the publication of a Journal of Immunology paper in 1995 by a team led by Shimon Sakaguchi, MD, PhD, who demonstrated that a marker on the cells’ surfaces could be used to pluck them from the crowd of all the other T cells.
“The main reason immunologists abandoned suppressor T cell research as a dirty science is that it was very phenomenological science and did not have a solid molecular basis such as a reliable marker specific for the population,” says Sakaguchi, who had worked as a postdoctoral scholar in Strober’s lab and is now at Kyoto University in Japan. He emphasizes that he — like Strober — was not interested in the cells per se, but in their ability to explain perplexing experimental results. “Once a reliable cell surface marker specific for such T cells was found, everybody now could see the cells.”
By that time, nobody wanted to call them suppressor T cells any more — to avoid the “bad press,” as Strober calls it, of their previous incarnation — so these days scientists call them regulatory T cells instead. Strober found that he was studying two types, now called natural killer T cells and CD4 Treg cells.
Even though regulatory T cells now solidly hold a place in the immune cell repertoire, there are more questions than answers. Questions such as: How many types of these cells exist? How can they be distinguished from other T cells? And how are they able to fine-tune the immune system to allow strong responses to pathogens but also to prevent autoimmune diseases and cancer?
Putting the cells to work
Despite the lingering questions, researchers are attempting to harness the peacekeeping abilities of these cells. Reducing graft-versus-host-disease is the regulatory T cell-based therapy that’s most advanced, primarily because the condition is deadly and current drugs to treat it are quite toxic, says Robert Negrin, MD, director of the division of blood and marrow transplantation. “Graft-versus-host disease is a disease that is worse than the leukemia or lymphoma the transplant is treating,” he says.
A Stanford team led by assistant professor of medicine Robert Lowsky, MD, began a clinical trial in 2002, translating Strober’s mouse studies to human cancer patients. “The beauty of this method is that the mechanisms are so well-understood in the animal model,” says Lowsky. “And what we see in humans appears to mimic what occurs in mice,” although the rarity of regulatory T cells in human blood makes it much harder to prove directly.
The team reported their results on the first 37 patients in 2005 in the New England Journal of Medicine. The Berkeley physicist Loken and nearly 100 more patients have since undergone the procedure. The protocol has recently become the standard for patients at Stanford Hospital & Clinics.
“Stanford was the ideal place for development of this study, for at least two reasons that don’t necessarily apply elsewhere,” says Paul Martin, MD, professor of oncology at Fred Hutchinson Cancer Research Center in Seattle, the nation’s largest blood stem cell transplant unit. “First is the Strober lab’s long-standing interest in regulatory cells and their potential use in blood stem cell transplantation. No other transplant team has had the benefit of such persistent effort in this arena.” And second, is the close working relationship between Stanford’s transplant teams and radiation oncologists.
Too good to be true?
The Stanford protocol combines localized blasts of irradiation and antibody treatments to tweak patients’ immune cells before they receive a blood stem cell transplant. In Loken’s case, the blood cells came from one of his sisters, who was an exact immunological match. On the day of his transplant, Loken received two bags of liquid in a procedure that, from his perspective seemed like an ordinary blood transfusion. After two weeks of recovery, he was back on a treadmill and stationary bike, ramping up to where he had been physically before leukemia struck.
“If such results prove to be universally reproducible, this study will definitely represent a sort of revolution in the field,” says Mohamad Mohty, MD, PhD, a blood cancer specialist at the Paoli-Calmettes Institute in Marseille, France, one of Europe’s largest cancer research centers. “At this point, one can ask why other investigators did not immediately adopt this protocol.” He and Martin cite as reasons the study’s small numbers of patients and relatively short follow-up, although patients like Loken are now years out with minimal problems.
Lowsky and Negrin have just launched a study with Kaiser Permanente of California, which will evaluate the outcomes of patients over 50 with acute leukemia who are treated with the Stanford protocol, compared with those who receive standard treatment. Larger-scale studies such as these — Kaiser provides care for more than 6 million people in California — will begin to answer the question of whether the procedure would work widely.
Only a large randomized study comparing patients who get the Stanford protocol with those who don’t will convincingly demonstrate the superiority of the Stanford approach, says Mohty, who soon hopes to be leading a European multicenter study of the protocol. “If such results become available, I cannot see investigators refusing the evidence,” says Mohty.
Loken, for one, has all the evidence he requires.
Comments? Contact Stanford Medicine at

