A quick look at the latest developments from Stanford University Medical Center
![]() Hi-ho stem cells
Hi-ho stem cells
![]() Thin-ebriated
Thin-ebriated
![]() National honor for Stryer
National honor for Stryer
![]() M.S. protection
M.S. protection
![]() Poop scoop
Poop scoop
![]() High tech is not enough
High tech is not enough
Hi-ho stem cells
Medical school researchers have found that human neural stem cells transplanted into the brains of rats and mice successfully navigate toward areas damaged by stroke.
The discovery and the new technique the researchers used to make it add up to encouraging news for researchers hoping to use stem cells to treat human neural disorders such as stroke, traumatic brain injury, Parkinson’s disease or radiation damage.
Salvatore Rubinno |
|
 |
|
The research group placed miniscule particles of iron inside stem cells to act as cellular beacons detected by magnetic resonance imaging. In fetal mice with brains still developing, the research group injected the stem cells into the fluid-filled regions called ventricles. From there, the iron-filled cells migrated along the path that stem cells normally take to populate the developing brain. Those stem cells then matured into the proper types of brain cells.
In adult rats that had a simulated stroke, the human stem cells migrated into the damaged region, matured into the appropriate type of neuron and support cells, and appeared to integrate into the surrounding tissue.
The only environment that rendered the neural stem cells immobile was the healthy adult rat brain. In the absence of any signals to beckon the stem cells, they stayed close to where the researchers implanted them.
The findings were published in the June 12 Proceedings of the National Academy of Sciences.
Senior author Gary Steinberg, MD, PhD, says the research also shows that the iron particles, called superparamagnetic iron oxide, don’t disrupt stem cells’ normal function. “This work is important because if a method of tracking the cells changes their biology, it will not be helpful,” says Steinberg, professor and chair of neurosurgery.
“We’re not saying we can treat patients immediately, but it’s a big step forward. This gives us considerable optimism for these cells,” he adds.
No one yet knows the best way to insert the cells, the ideal conditions for cell survival or the optimal timing after an injury for transplanting the cells. But now that they have the ability to monitor where the human stem cells go in real time, researchers can compare different techniques to learn what works best. — AMY ADAMS
The work was funded by the National Institute of Neurological Disorders and Stroke, Russell and Elizabeth Siegelman, the William Randolph Hearst Foundation, Bernard and Ronni Lacroute, and the Swiss National Science Foundation.
| ![]() Back
to Top |
Back
to Top |
Thin-ebriated
An Oprah Winfrey-inspired study at Stanford has found that patients who undergo gastric bypass surgery to lose weight will get drunk faster and take longer to sober up.
Salvatore Rubinno |
|
 |
|
About 150,000 Americans a year undergo this surgery, which reduces the stomach to the size of a walnut so that patients can eat only about an ounce of food at a time.
“It may sound strange, but Oprah really did inspire this study,” says John Morton, MD, assistant professor of surgery and senior author of the study, which will be published this fall in the American Society for Bariatric Surgery’s journal, SOARD.
An October 2006 episode of The Oprah Winfrey Show explored possible dangerous effects of alcohol on patients who had undergone gastric bypass. In the ensuing weeks, Morton says, “I got question after question from patients asking, ‘What happens when I drink alcohol?’”
Morton has performed more than 1,000 gastric bypass surgeries and routinely cautions patients about drinking alcohol after the surgery. The patient concerns arising from the Oprah episode sent him looking for hard data on the issue. When he found very little, he decided to undertake his own study.
“I’ve heard the anecdotes of a patient who will drink one glass of wine and get a DUI, but I wanted to know if there is really a difference before and after surgery,” Morton says.
To measure the effects of alcohol, researchers gave 19 post-operative gastric bypass patients and 17 control subjects 5 ounces each of red wine. They drank their wine within 15 minutes. Breath-alcohol levels were then measured every five minutes until levels dropped to zero.
The gastric bypass patients reached a breath-alcohol peak of 0.08 percent, while the control group’s level peaked at 0.05 percent. The bypass patients also took significantly longer to return to zero, averaging 108 minutes versus 72 minutes for the control subjects.
“The bypass patients have a fundamentally altered alcohol metabolism,” Morton says.Gastric bypass alters several physiological functions that could explain this change, in particular a decrease in the enzyme most responsible for alcohol metabolism.
“Patients have to be careful with alcohol,” Morton says. “They’ll become tipsy a lot easier.” — TRACIE WHITE
| ![]() Back
to Top |
Back
to Top |
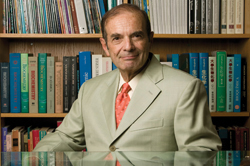
National honor for Stryer
Neurobiologist Lubert Stryer, MD, has received the nation’s highest scientific honor, the National Medal of Science, for his achievements in a wide range of fields that include the development of a DNA chip used in genetics.
Steve Gladfelter/VAS |
|
 |
|
Stryer, the Mrs. George A. Winzer Professor of Cell Biology, Emeritus, was one of eight scientists to receive the 2006 award announced this summer.
“Lubert Stryer is a true legend as a scientist and scholar whose name also is known to students of biochemistry because of his classic book on this topic,” says Philip Pizzo, MD, dean of the medical school.
Although best known for developing a gene chip and for writing a biochemistry textbook, Stryer, 69, also made major contributions to diverse areas of medicine. His research over four decades has dealt with the interplay of light and life. He made landmark contributions to understanding proteins on the molecular level through fluorescence spectroscopy techniques. He also helped explain how the eye’s retina processes light.
“Lubert Stryer is one of the last Renaissance men in biomedical research,” says Tobias Meyer, PhD, a Stanford professor of chemical and systems biology who did postdoctoral work under Stryer. “He combines a broad knowledge of science with amazing communication skills and an ability to translate his research discoveries into practical applications.”
The highest profile product of his work, the microarray “gene chip,” took root during his 1989 leave of absence from Stanford to help found Affymax, a therapeutic drug discovery company in Palo Alto. Stryer helped develop a method for efficiently generating the thousands of distinct com-pounds arrayed as individual spots on each chip. This method is still used by Affymetrix, the Santa Clara company later spun off from Affymax, to make gene chips.
Stryer first came to Stanford in 1963 as an assistant professor of biochemistry. “I had the good fortune of being nurtured by Arthur Kornberg, Paul Berg, Robert Baldwin and other members of that remarkable department,”‘ he says. He later left for a seven-year stint at Yale, returning to Stanford in 1976 as the first chair of the Department of Structural Biology. His interests shifted to neurobiology, where he is currently an emeritus professor.
At each juncture of his career, Stryer contributed to leaps in knowledge.
He developed what he termed “a spectroscopic ruler” — a method of measuring which atoms are neighbors and how far apart they reside in large, complex protein molecules using fluorescence — that is used in thousands of labs.
But perhaps his biggest impact has been his textbook Biochemistry, now in its sixth edition, which has inspired thousands of students to pursue biomedical research themselves. — MITZI BAKER
| ![]() Back
to Top |
Back
to Top |
M.S. protection
The same protein that triggers the spiral of damage in multiple sclerosis can stop the attack cold.
This protein — alphaB-crystallin — is normally found in the lens of the eye, but it develops in the brain and spinal cord in response to the injuries inflicted on nerve cells by M.S. The nerve-cell injuries can cause people to suffer loss of motor control and even paralysis.
Scientists have known since 1995 that this protein builds up in M.S. patients’ brains, but its function was a mystery. Now Lawrence Steinman, MD, professor of neurology and neurological sciences, and his team have demonstrated the protein’s protective role in a mouse model of multiple sclerosis: When injected into mice, it can reverse paralysis.
They published their findings in the July 26 issue of Nature.
In multiple sclerosis, the immune system launches an attack against the myelin sheath surrounding nerve cells, causing them to misfire.
For reasons not yet understood, the immune system considers the expression of the alphaB-crystallin protein in the brain a danger signal and attacks this healing substance as well. But injecting this same protein into mice with M.S. symptoms reversed the paralysis.
Once Steinman’s team had a grasp of what was occurring in mice, they turned to humans. Using a collection of spinal fluid samples, Steinman’s team tested them on their antibody arrays spotted with minute amounts of hundreds of myelin sheath proteins to provide a profile of the antibodies’ targets.
They found that in humans, too, the highest antibody response was directed against alphaB-crystallin, leading the researchers to speculate that the protein could possibly reverse the damage in humans as it does in mice.
“I am going to strenuously work to bring this from our benches to the bedside,” says Steinman, “through collaborations with existing companies — or we will start a new one.” — MITZI BAKER
This work was funded by the National Institutes of Health, the National Multiple Sclerosis Society and the Multiple Sclerosis Society of Canada.
| ![]() Back
to Top |
Back
to Top |
Poop scoop
Researchers at the School of Medicine are as interested in a baby’s poop as doting parents are, and for good reason. The team has made the most extensive survey yet of the virtually uncharted territory of the baby’s gut.
Salvatore Rubinno |
|
 |
|
“It’s an amazing thing trying to figure out how we go from having a completely sterile gut to a microbial ecosystem that will be with us for the rest of our lives,” says senior author, Patrick Brown, MD, PhD, professor of biochemistry. “What could be more fundamental than that?”
The findings were published in the July Public Library of Science-Biology.
Looking at stool samples from 14 healthy infants over their first year of life, including a set of fraternal twins, researchers found that each baby had very different microbes colonizing their intestinal tracts at different stages.
A baby’s gut is a rapidly evolving place. In the beginning, it has no inhabitants. But within days of a baby’s birth, the microbial immigrants establish a thriving community whose population soon outnumbers the baby’s own cells tenfold, a ratio that persists throughout life.
“It’s really striking, the degree to which the patterns of bacterial abundance were so dynamic over time,” says collaborator David Relman, MD, associate professor of medicine and of microbiology and immunology. “Things suddenly drop in abundance, and other things appear and take their place.”
Six of the 14 babies had some course of antimicrobial medicine during their first year. Only one baby had an extremely dramatic change in the microbial community in response to the drugs.
The study included one set of fraternal twins, who had the most similarity in their microbial community profiles, leading to speculation about the combined effects of genetics and environment. The similarity between the twins “gives us a glimmer of hope that it’s not a completely chaotic process,” says lead author Chana Palmer, PhD, a former graduate student in Brown’s lab. — MITZI BAKER
This work was supported by funding from the Horn Foundation, the National Institutes of Health and the Howard Hughes Medical Institute.
| ![]() Back
to Top |
Back
to Top |
High tech is not enough
Health-care management leaders tout electronic health records as a key element in improving the effectiveness and efficiency of U.S. medical care, but a recent study found that electronic records were not associated with improved quality of outpatient health care in 2003 and 2004.
Of 17 quality indicators assessed by the study, electronic health records made no difference in 14 measures. In two areas, better quality was associated with electronic records, while worse quality was found in one area.
“We need to be cautious about the assumption that electronic health records are going to solve problems around health-care quality by themselves,” says senior author Randall Stafford, MD, PhD, associate professor of medicine at the Stanford Prevention Research Center. “It’s not sufficient to have an electronic health record system that provides readily available patient data and decision-making guidance. Physicians have to be receptive to that input and willing to act on that input.”
The 14 quality indicators for which electronic records made no significant difference included prescribing recommended antibiotics, diet and exercise counseling for high-risk adults, screening tests, and avoiding potentially inappropriate prescriptions for elderly patients.
In two quality areas — not prescribing benzodiazepine tranquilizers for patients with depression, and avoiding routine urinalysis during general medical exams — doctors using electronic record systems fared better than those who didn’t.
But when it came to prescribing statins for patients with high cholesterol, physicians using electronic systems did worse.
Stafford and his colleagues drew the data for their study from the National Ambulatory Medical Care Survey, which provides information on patient visits to office-based physician practices. They published their findings in the July 9 issue of the Archives of Internal Medicine.
The researchers found that electronic health records were used in 18 percent of the estimated 1.8 billion physician visits that occurred in 2003 and 2004. Using a previously defined set of 17 quality indicators for ambulatory care, the researchers checked the database to determine whether an electronic health record system enhanced the quality of care.
Stafford has a couple of theories as to why electronic health record systems failed to boost the quality of care. First, in 2003 and 2004 doctors might have been using older systems that did little more than transfer information from the paper record into electronic form. Many of the more soph-isticated systems available today, however, can recommend the types of medications or tests that might be best-suited to a patient’s condition.
Which brings up the second theory: No matter how sophisticated the system, it can’t dictate a course of action to a physician, Stafford says.
“We’re still on a learning curve in terms of how physicians relate to electronic media,” he says. “Recent graduates of medical school are clearly more comfortable with these technologies, and they’re only gradually diffusing into the whole of the medical practitioner population.” — SUSAN IPAKTCHIAN
The study was funded by the U.S. Agency for Healthcare Research and Quality.
| ![]() Back
to Top |
Back
to Top |
Comments? Contact Stanford Medicine at

